5 Clinically Proven Remedies to Tackle Gut Heath Issues
Part II of a 2-part series on The Hormone-Gut Cycle
Five researched and recommended remedies you can start incorporating now into your daily routine to get your gastrointestinal (GI) health in order while also addressing stress and weight gain around the mid section.
#1. Take a daily probiotic
Probiotics help with GI issues like gas, irritable bowel symptoms, bloating,and constipation, and may also help with upper GI symptoms such as acid reflux. The good bacteria found in a probiotic stimulates the digestive hormone cholecystokinin, and helps with excretion and toxin elimination allowing you to pass stool with ease and regularity.
A product I recommend and have been taking regularly is Routine. There are three ingredients that have been proven in clinical studies to promote better digestion and significantly reduce the occurrence of GI issues. Bifidobacterium lactis B-420 and HN019 to populate the gut microbiome with beneficial bacteria, and Bifidobacterium lactis BL-04 to strengthen the immune response. Probiotics are also well known to address weight problems. One ingredient in particular, Christensenellacea, works to reduce waist circumference and body mass, and boosts metabolism. A second stain contained in Routine called Lactobacillus3 helps regulate weight. Routine also includes ashwagandha, a calming adaptogen, known to help ease stress and anxiety, which is discussed in greater detail below.
#2. Practice stress management.
As mentioned in Part I of this series, the parasympathetic nervouse system (PSNS) is our rest-and-digest nervous drive. When activated, our heart beat calms down and our digestion is stimulated. PSNS should be our dominant state when we are not in danger as it allows the body to maintain homeostasis, a state where all systems are balanced and the body and brain are able to perform optimally. Stressors or perceived stressors act as stimuli that threatens our homeostatic processes and triggers the fight-flight-freeze sympathetic nervous system (SNS) drive.
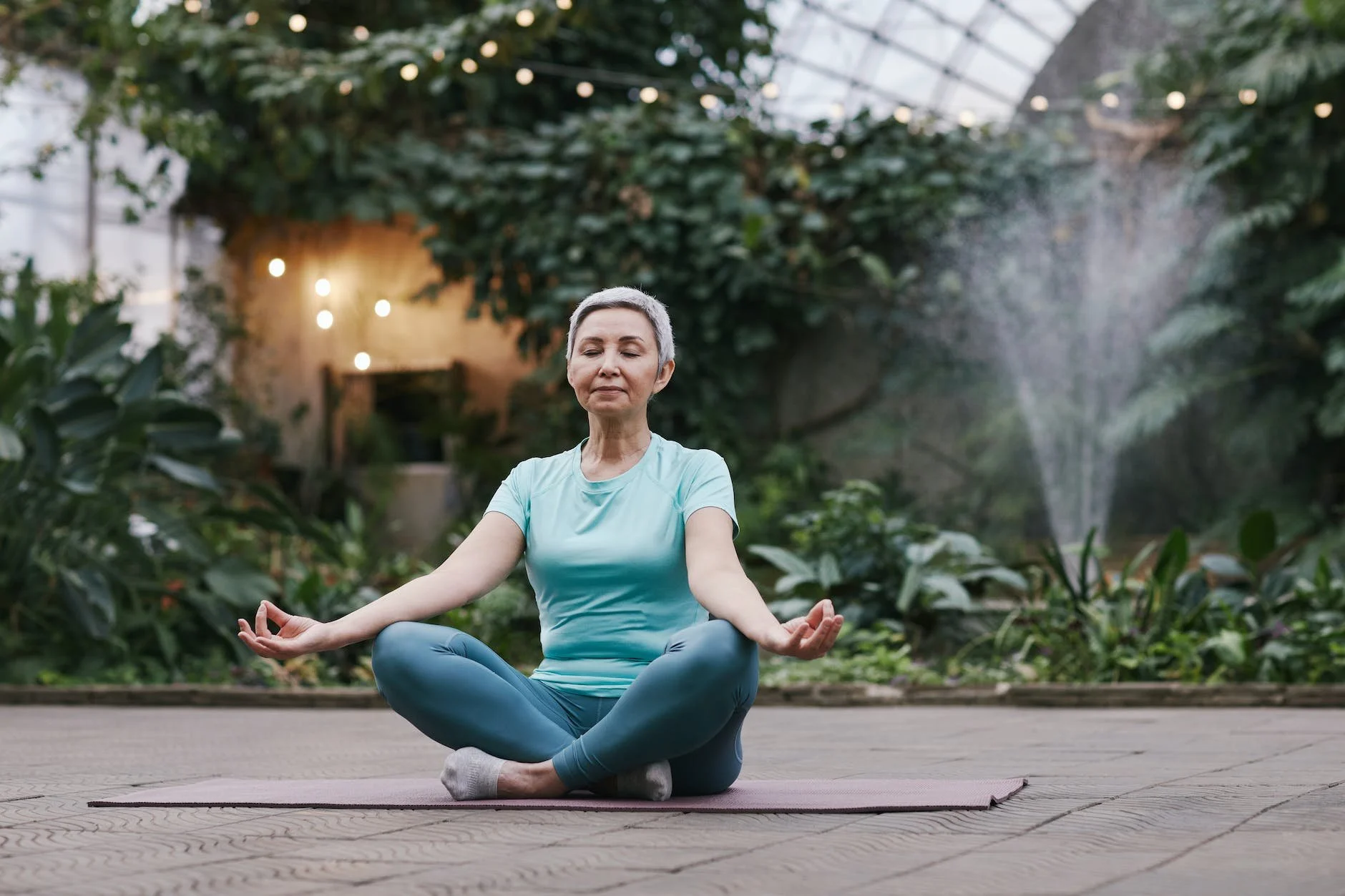
Yoga, mindfulness, and meditation are all practices which signal the nervous system that the body is safe. Deep breathing and other breathwork techniques can also tell the brain and body that we are safe and not in any form of danger. Of course, for the effects to be long lasting and habitual, stress management practices should be a lifestyle routine rather than a quick fix.
Watch for future articles and offerings on still and moving meditation for menopause!
#3 Track food sensitivities
Foods we once enjoyed before menopausal transition and never caused problems can suddenly wreak terrible havoc on our digestive system. Falling estrogen levels will have an effect on our gut mobility, which is defined as the slowing down of digestion from consumption to elimination. This sluggishness has a high potential to invite more bacteria into the digestive tract because the food is in the system longer and fermenting, thus leading to bloating, gas and possibly constipation.
Keeping a food journal and recording not only what you eat, but when and how will help pinpoint problematic foods. Time of day or the timeframe between your last meal and going to bed is also worth noting. How you eat is also a key indicator. For instance, rushing and not taking the time to enjoy the meal, eating in front of a TV or computer screen, or eating past feeling satiated can lead to digestion problems. One of the reasons is that speed-eating does not allow the food to be broken down with the saliva in the mouth, which aids the digestive process. As a result, this places more demand on the intestines to break down food.
For more on the digestive process visit the Mayo Clinic and watch the slide show in the digestive system.
It’s also worthwhile to track how you react to certain foods with the changing hormones by taking a food sensitivity or food intolerance test. What's the difference between food allergies and food sensitivities? Check out this article by Biostation. Consult with a naturopath to learn more about getting tested.
#4 Intermittent fasting
The jury is definitely out on this common yet confusing strategy. If you are active on social media you will have seen countless posts about how beneficial intermittent fasting (IF) is for controlling GI issues and tackling the jelly belly. Time restricted eating (TRE) is a type of IF which is the focus in this article.
Here’s how it works and why?
A TRE type of fast means your eating window is limited to a specific time of day without consuming food during the night. An ideal ratio, recommended in her bookThe Galveston Diet by Dr. Mary Claire Haver, is 16:8. The time without food is 16 hours. So, for example, if you have your last meal of the day at 7 pm, you break the fast at 11 am and only consume food for an eight hour period.
There’s a growing body of research that concludes IF is “a cleansing activity” because it helps balance the composition of the gut-microbiome, which, in turn, has many positive effects on all tissue and organ systems. While research is still advancing in this area, studies are finding that limiting the eating window and restricting food intake during the night supports our circadian rhythm. During the night, our metabolic responses to glucose slow down, therefore, making it plausible that a chronically disturbed circadian rhythm may affect gastrointestinal function and impair metabolism and health.
IF also results in consuming fewer calories and slightly boosts metabolism, making it a very effective strategy for weight loss, particularly visceral fat, the fat that is stored in the abdominal cavity. These results are achieved because IF lowers insulin levels, increases human growth hormone (HGH) levels, and increases norepinephrine (noradrenaline), all which work to convert body fat into energy.
#5 Use adaptogens
Adaptogens are a class of medicinal or therapeutic plants that increase the body’s resistance to stress by targeting the hypothalamic-pituitary-adrenal (HPA) axis, a neuroendocrine system that controls your reaction to stress and regulates various body functions, such as digestion, mood, temperature control, and immunity.
As mentioned earlier, the rise in the stress hormone cortisol slips us into a fight-or-flight sympathetic drive. With menopause, coupled with stresses of modern life, women spend a large percentage of time in this state. Use of adaptogens over time blocks some of our cortisol response and, therefore, the experience of the stress is lessened. Cortisol release will remain the same for the most part but our reaction to it changes.
There are two classes of adaptogens, stimulating and calming. Two calming adaptogens that work on calming reaction to cortisol are Ashwagandha & Holy Basil.
Ashwagandha, known in botany as Withania somnifera, turns down your fight or flight response and can help decrease anxiety and depression. In some clinical trials, it was found to reduce cognitive impairment (brain-fog), fatigue, and cholesterol, as well as address body composition because of its blood glucose control properties. However, it is contraindicated with thyroid and immuno-support medication. So, if you are on such medication, Ashwaganda is not recommended.
Holy Basil (Tulsi), a sacred Indian herb, is also a calming adaptogen used to improve energy and immunity, reduce fatigue, and lower blood glucose levels. As well, Tulsi works as a relaxant by reducing cortisol. There is a wealth of other benefits to be had with Tulsi including its anti-inflammatory, antioxidant, analgesic (painkiller), and anti-cancer properties.
Adaptogens are supplements, which is an area of holistic medicine largely unregulated. Less is best when it comes to adaptogens. Seek quality products and speak to a nutritionist or naturopath for recommended daily dosage and duration.
*This article is an accumulation of information gathered from many sources and is for information purposes only. It does not constitute medical advice nor does it replace professional medical diagnosis. Always consult with your family doctor or a healthcare professional about your menopause symptoms, digestive health and any prolonged abdominal pain you may be suffering from.
The Hormone-Gut cycle is complicated and complex. The more you understand how the aging process impacts our gastrointestinal health and why, the wiser you become in addressing it effectively.
Knowing what is going on with your gut sets you up for success in choosing remedies to alleviate these ongoing issues while also addressing stress and weight gain.
Emme Elle Coaching is offering a Trust Your Gutonline mini-course that explains the science of our hormones as they relate to the gut microbiome and how you can get it back on track.
Pre-register now and save $10. Course launch date Nov 1, 2023. Your price including the workbook is $29 USD. Get on the list before this offer closes!
References